Welcome to Ripple Effect
I am hoping that this will be a journey that opens your eyes and you have that light bulb moment where it all suddenly makes sense – feel free to come back to this first part at any time and then do share what your light bulb moment was …
I can assure you that this will equip you with the knowledge that you need in order to navigate the Journey ahead of meeting your baby(ies) and welcoming them earth side … just think on this … this little soul chose you as their parents … isn’t that wonderful and so sacred … your journey should be honoured … So here goes let’s jump in and explore everything you need to know.

Pre-course reading – Dani Diosi’s Hypnobirthing – Breathing in Short Pants … this book can be ordered from Amazon either in paperback or electronic format.
Complete the client questionnaire download from here: ripple effect pre-course questionnaires and email it back to me via rippleeffectyoga@hotmail.com
Ask any questions you may have ….

Women are born with the ability to give birth to their babies.
PHYSICAL FUNCTION just like breathing, digesting food, eliminating waste and our heart beating.
Our bodies already ‘know’ how to do it.
- Physiological birth – feel the contractions for specific reasons,
- Feel your baby’s head crowning for specific reasons,
- Understand the effect the contractions have on your baby is for specific reasons,
- The bodily fluid the baby comes into contact with on their way out, is for a very specific reason.
- There are no design flaws.
Birth sometimes develops complications which could require medical intervention.
Unfortunately, modern society and the history of fear surrounding birth have an extremely negative affect on how people view labour and that’s where ‘hypnobirthing’ comes into its own.
Independent Midwife and hypnobirthing instructor, Kemi Johnson described it as “a way of introducing women to the concept of choice surrounding their births.”
Instilling confidence in the physiology of birth provides the foundation upon which everything else is built.
So however you’re planning on giving birth, you may find it useful to understand the roles our different body parts play in the overall process.


- What the contractions actually are
- What contractions specifically do
- The different stages of labour
- The birthing hormones which support, nurture and guide the birth from pre-labour, during actual labour and through to the post-partum period.
- The pain relief options
- The interventions ‘offered’ BUT these may not be YOUR only option
- The decision making process which may help you should a decision need to be made.
- How all the techniques you’ll learn can be used even when birth becomes or starts off as ‘medical’.
Fear of the name = Fear of the thing
VAGINA CONTRACTIONS

The female body is amazing
To accommodate the growing foetus (baby) the intestines and organs move out of the way.
The stomach muscles separate as the baby grows
Constant toilet trips
Eating small amounts
May feel a little breathless

An impressive organ
POWERFUL STRONG
CAPACITY TO GROW
“KNOWS” what to do when there is a baby growing inside it and it knows how to get that baby from the inside to the outside ….
Small, pear shape set of muscles
when not pregnant nestles within the pelvic girdle.
It has three main areas:
The Fundus – which is the layer of muscle at the top of the womb.
The Body – the main chamber where the baby grows and develops.
The Cervix –narrow channel of circular muscles, linking the cervix to the vagina. The cervix has an opening at the bottom for sperm to go in and babies to come out
There are three layers to the uterus:
The Perimetrium – a thin lining connecting the uterus to the body lining.
The Myometrium – a thicker middle muscular layer covering the outside of the uterus, located between the perimetrium and the endometrium. The muscular nature of this layer is extremely important for the contractions needed for childbirth.
The Endometrium – the thinner, inner layer of the uterine wall which builds up every month, preparing for the fertilised egg implantation. When that doesn’t happen the lining sheds, causing the monthly period.
The Myometrium (middle layer of the uterus) has three different layers of muscle within it.
Each has a different role to play during labour
Don’t you just love the power of 3 …
All work in harmony when birthing your baby
The outer layer has longitudinal muscle fibres that go down the front and back of the uterus, with the main mass of muscle being at the top. As this layer of muscles contract, they gently push up the circular fibres of the inner layer causing the cervix to dilate (or open) and extra muscle mass to gather at the top of the uterus (the fundus). When the cervix is open enough to allow a baby’s head through (usually considered to be around 10cm) the motion of these longitudinal muscles changes, allowing the extra muscle thickness at the top of the fundus to act as a piston to push the baby out of the uterus and down the birth canal. The middle layer is a mass of muscle fibres all matted together forming figures-of-eight around the uterus’s blood vessels. When these muscles are relaxed the blood flows freely, enabling the baby to receive all the oxygen and nutrients she needs. When they contract, the blood vessels are constricted, temporarily reducing the flow of blood etc. to the baby.
This may sound scary but this process is actually helping prepare their lungs for life outside of the womb. This restricting of blood flow is also very important because it allows the safe release of the placenta with minimal bleeding. The inner layer consists of circular fibres that go around the uterus, with the main mass concentrated in the lower segment close to the cervix. Their role during pregnancy is to keep the cervix closed and the baby safe.
Interestingly, when this layer contracts during childbirth, it keeps the cervix closed and can therefore stop or slow down the function of the uterus. This usually will only happen if the mother feels threatened or unsafe in any way.

The cervix sits at the bottom end of the uterus. 
If you have felt inside your vagina you know that the hard, nubby bit is the Cervix.
During your menstrual cycle it’s position will change
During pregnancy, it stays firmly closed with a plug of mucous in the opening (the external os) to prevent any infection from travelling into the uterus. This plug will come out in the days, hours, minutes before the mother goes into labour and the cervix begins to soften.

 The long muscles of the uterus reach down, gradually pull back on the circular muscles of the cervix these are felt as contractions.
The long muscles of the uterus reach down, gradually pull back on the circular muscles of the cervix these are felt as contractions.
They are softening & shortening the cervix (effacement) pulling it into the body of the uterus (dilation) until it’s open wide enough for the baby’s head (approximately 10cms)
Internal examinations are a choice they are NOT compulsory.
They give you a snap shot of what is happening at that moment in terms of progress and where you are in the process.
Hospital guidelines suggest a woman’s cervix will dilate ½ cm/hour.
Cervical dilation is not the only indicator and things can change so rapidly with babies being born a few contractions later or taking their own sweet time.
Most hospitals would be unwilling to admit a woman until the cervix is at least 4cm – 5cm dilated because it is only then she is deemed to be in ‘active labour’ (although there is new research which suggests women are not in ‘active labour’ until the cervix is 6cm dilated – Sarah Wickham, 2018).
Unfortunately, despite this form of measurement being extraordinarily inaccurate, it has become the ‘norm’ for assessing a woman’s labour.
Just as with a photograph, you can’t say what happened just before the photo was taken and you can’t say what’s going to happen after. Therefore, ascertaining the cervical dilation at a particular point, doesn’t really give a lot of information. I have been at births where it has taken the mother ages to get to 3cm but 2 or 3 contractions later she is holding her baby in her arms. Similarly, one mother I was with was at 9cm and there was no baby for another 7 hours.
If mother and baby are fine and healthy there should be no pressure to rush the process.
Every woman is different … and so are their cervix’s!
First time mothers will generally take longer to get to that ‘magic’ 4cm – 5cm because the contractions need to bring their cervix forward (it’s posterior during pregnancy i.e. pointing backwards), then soften it and then open it. So even if you’re examined by a midwife and told you’re ‘only’ 2cm dilated, remember that your uterus has already done a fantastic amount of work to get to that point, and you should be feeling rather chuffed with yourself that you’ve reached that stage. There is a fantastic You Tube video doing the rounds lately, involving a balloon and a ping pong ball (Google it, the woman who posted it is called Liz Chalmers) which demonstrates exactly how much work the uterus has to do before it can even start. Second time mothers generally (although not always) tend to have quicker labours because their bodies know what to do if they have reached full dilation before, due to muscle memory. The labour hormone receptors also tend to be more efficient.

The circular muscles usually prevent labour & keep something in until it is time to let them go. E.g. cervix, bladder and anus
Ina May Gaskin (author of Ina May Gaskin’s Guide to Childbirth) discovered a very important rule relating to these muscles.
They prefer an atmosphere of intimacy and privacy
They don’t respond to ‘Push!’ or ‘Relax’.
Everything can close down if that person becomes upset, frightened, humiliated or self-conscious.
Why? High levels of adrenalin
The state of relaxation of the mouth and jaw is directly correlated to the ability of the cervix, the vagina and the anus to open to full capacity. (2003) Sphincter muscles simply do not open under stressful conditions.
The circular muscles around the cervix usually prevent labour from happening.
Sphincters, such as the cervix, bladder and anus are round circular muscles designed to keep something in until it is time to release it.
The renowned Ina May Gaskin (author of Ina May Gaskin’s Guide to Childbirth) discovered a very important rule relating to these muscles: Excretory, cervical and vaginal sphincters function best in an atmosphere of intimacy and privacy – e.g. a bathroom with a locking door or a bedroom, where interruption is unlikely or impossible.
These sphincters cannot be opened at will and do not respond well to commands such as ‘Push!’ or ‘Relax’.
When a person’s sphincter is in the process of opening, it can suddenly close down if that person becomes upset, frightened, humiliated or self-conscious. Why? Because high levels of adrenaline in the bloodstream do not help, in fact sometimes actually prevent the opening of the sphincters.
The state of relaxation of the mouth and jaw is directly correlated to the ability of the cervix, the vagina and the anus to open to full capacity. (2003)
This is a great video that shows you the power of observation and pressure on a couple not only to conceive but to birth within the establishment.
https://youtu.be/lZG0T7xHy6A

The birth canal and the vagina are one and the same thing
This ridged passage runs from the neck of the womb to the outside wall of the body and is made up of multi-folded skin which facilitates the canal to open to many times its normal size.
It is about 7.5 cm long at the front and about 10cm long at the back with a couple of lubricating glands on either side which help keep the area moist and slippery during both child birth and making love.
The area is covered in lots of very tiny blood vessels so even if there is a damage to it or a tear the actual blood loss will be minimal as the vessels are so small.
Once the cervix has opened fully, the ridges in the vagina (normally there to create pleasure during sex) flatten out and become excessively lubricated to help the baby to be born.

 The pelvic floor consists of 3 layers of muscle, ligaments and connective tissue.
The pelvic floor consists of 3 layers of muscle, ligaments and connective tissue.
Essentially it’s a ‘hammock’ holding everything in place.
It stretches from the front (pubic bone) to the back between the legs (sacrum and coccyx.) 
The PUBOCOCCYGEUS (main muscle PF) wraps itself around the openings of the urethra, vagina and anus in a figure of eight.
During pregnancy, due to the increased weight of carrying a human these muscles will work very hard.
These muscles need ELASTICITY and this is the focus engaging and connecting how to release them.
As the baby is being birthed (crowning) it’s important for women to be as relaxed as it possible …
YOU are in great hands with THE PELVIC FLOOR QUEEN!
There are lots of lovely positions to connect with your pelvic floor and to feel that release … we will practice these so that you are aware of what you need to do.
Having an epidural can change the tone of the pelvic floor, giving the baby nothing to rotate against.
This is one of the reasons why an epidural can increase the chances of needing an instrumental delivery (i.e. forceps, ventouse or in some cases a caesarean.)
Video – epidurals TO BE ADDED
Pelvic floors – pregnancy – we will go over these in the sessions.
Pelvic floors – postnatal we will discuss what these are and when they can be started dependent on how your birth goes.
‘horse breath’ – loose jaw and mouth, reflect the state of the muscles in the cervix and pelvic floor. A great practice that helps you to identify if you are holding tension. We will do this in the sessions.
As the baby’s head (or any presenting part) meets the resistance of the pelvic floor, it enables that part to rotate forward until it comes to lie under the symphysis pubis (known as Hart’s Law). In other words, the tone of the pelvic floor enables the baby’s head to extend (they usually have their chins tucked into their chests so their heads fit neatly in the pelvis) enabling birth.

The pelvis which supports the weight of the body through the spine; it is a bony cradle.
The baby’s head will move (engage) into the pelvis from roughly 36 weeks for a first baby
Any time up until, sometimes during labour for second and subsequent babies.
The baby’s head, shoulders and body need to pass through this circle of bone in order to be born.
You will only grow a baby that is appropriate to you
Cephalopelvic disproportion (i.e. baby can’t fit) can happen in cases of injury, disease, malnutrition or gestational diabetes, but it is extremely unlikely.
‘My last baby was far too big for me so I had to have a Caesarean’,
‘Thank goodness the obstetrician was there to save us, I would never have been able to get that baby out.’
More likely due to the circumstances of the births, such as position, choice of pain relief, intervention, etc. rather than a super-size baby.
In fact, several studies have shown it is the suspicion of a big baby, not big babies themselves that leads to complications because of the way women are subsequently treated (Decker and Bertone, 2019) It is also impossible to tell the internal proportions of a woman’s pelvis by looking at her.
Petite women can and do give birth to 10lb baby’s without so much as a graze! The fact of the matter is, our babies are far more likely to weigh upwards of 7-8lbs than under. Our babies are getting bigger because we are.
If you have visited heritage buildings you may have noticed that some of the doorways were low because the people were smaller.

You’ll have been told about the ‘optimal’ baby position, head down, spine facing the front of the mother’s tummy and slightly to her left (Left Occiput Anterior (LOA).
If the baby is in any other position that’s absolutely fine … let’s explore this a little further …
 Babies can turn posterior (back to back) during labour even if they were anterior (spine facing forward towards the mother’s front) when the mother began her labour.
Babies can turn posterior (back to back) during labour even if they were anterior (spine facing forward towards the mother’s front) when the mother began her labour.
Babies change position and move throughout labour because they are constantly trying to find the best way out.
Lower back pain when the baby is descending through the pelvis –it’s a misconception that if there’s back pain the baby must be back-to-back.
Labour can be long or quick regardless of what position YOUR baby is in.
Understanding how the baby needs to navigate the pelvis is really helpful got you to understand which positions would be supportive and helpful.

Sitting on a birth ball, bouncing up and down, swaying from side to side helps encourage the baby into a good, head down position, whilst toning the ligaments supporting the uterus.
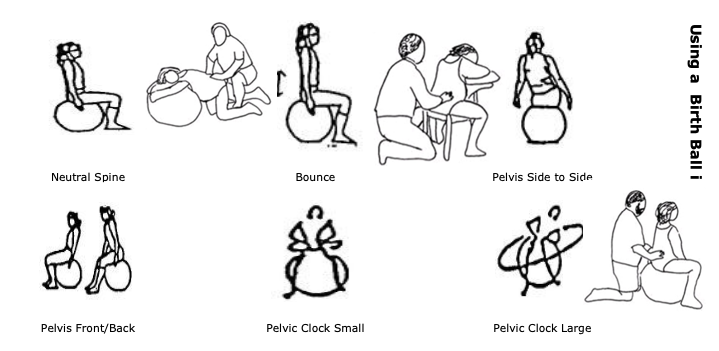
Sitting on a chair the wrong way round, or being in an all four’s position, either on hands and knees or leaning over the ball. FYI – all the positions are also excellent for labour!
www.spinningbabies.com offers optimal positioning techniques that may be useful during YOUR pregnancy and also during labour

Being in an upright, open, forwards position avoiding being on YOUR back which requires YOUR baby navigating a curve in the birth canal. This is hard work. YOU want gravity to help.
Being on your back restricts the sacrum and coccyx to do it’s magic. The coccyx needs to move out of the way, so the baby can pass through.
At the end of the day … listen to YOUR body – it knows where it’s comfortable & what works for you.
Exploring various positions. See the diagrams
These photos may help to understand

 The top of the baby’s skull is made up of several bones connected by flexible membranes. These membranes or fontanelles can be seen as ‘soft spots’ on top of the baby’s head and their purpose is to enable the bones to move and slide over each other so the head becomes moulded as it moves down the birth canal.
The top of the baby’s skull is made up of several bones connected by flexible membranes. These membranes or fontanelles can be seen as ‘soft spots’ on top of the baby’s head and their purpose is to enable the bones to move and slide over each other so the head becomes moulded as it moves down the birth canal.
Regardless of size the head will mould.
Vaginal babies often have cone shaped heads when they are born because of this bone movement
Caesarean babies heads are usually much rounder because they haven’t come through the birth canal.

 Develops from both the mother and the baby,
Develops from both the mother and the baby,
Embeds itself into the uterine wall
Attaches to the baby via the umbilical cord, however there is no mixing of maternal and foetal blood. This is because the maternal blood is at a much higher pressure. If the baby was connected to his mother’s circulatory system, his blood vessels would burst.
The foetus and the mother can, however, have different blood groups, but you would know about this if this was the case. (Rhesus Negative/Positive).
know about this if this was the case. (Rhesus Negative/Positive).
The mother’s blood flows into the spaces in the placenta and the baby’s blood is carried by the umbilical artery into villi, capillaries that project, ‘finger-like’, into the placental space.
Creates a large surface area of a thin barrier between the two circulations, enabling essentials for healthy growth, such as oxygen and nutrition to enter the baby’s blood system by diffusion.
In turn, the baby needs to dispose of waste – the carbon dioxide being constantly produced in all their cells, as well as the amniotic fluid which is drunk and then excreted. This waste passes through the thin walls of the villi into the mother’s circulatory system and she gets rid of it.
Through this method of exchange, the baby is also given the mother’s antibodies, providing immunity to a host of bacteria it hasn’t even come into contact with yet. However, drugs can also cross the placenta, which is why it is so important mothers avoid these during pregnancy.
 During the 3rd stage of labour the placenta is birthed.
During the 3rd stage of labour the placenta is birthed.
Amazing organ.
You may have the chance to look at it or you may be encapsulating it. Around the size of a dinner plate, approx. 3cm thick and reddish blue in colour with two types of membranes attached to it – the amnion (filled with fluid) which surrounds the baby and the chorion which in turn surrounds the amnion. The baby’s side of the placenta is relatively smooth whilst the side that has been attached to the uterus has lumps and bumps of arteries and veins running across it.

The umbilical cord connects the placenta to the baby it’s THEIR lifeline.
A vein carries oxygen-rich blood and nutrients from the mother to the baby, and 2 arteries that return deoxygenated blood and waste products from the baby through the placenta for the mother’s body to eliminate. These blood vessels are surrounded by a sticky substance called Wharton’s Jelly which prevents the umbilical cord from forming too tight a knot. The umbilical cord continues to transfer oxygenated blood, making sure the baby has enough oxygen whilst their lungs are starting to expand (this happens as soon as the baby feels a change of temperature on his skin).
The cord contains a third of the baby’s blood volume.
The cord blood contains vital vitamins and stem cells which should be transferred into the baby. Hence delayed cord clamping & massaging from mum to baby.
NICE (National Institute of Clinical Excellence) guidelines support DCC and in an ideal situation, cord cutting would wait until the cord stops pulsating and changes colour from purple/blue to white.

Amniotic fluid (a clear liquid) surrounds the baby whilst it is in the womb.
Protects
Shock absorber
Helps maintain the baby’s temperature
 Gives it the space and ability to move around which enables bone development.
Gives it the space and ability to move around which enables bone development.
The mother’s body makes amniotic fluid all the time although the levels surrounding the baby change constantly as it drinks and then wees. Around the time the baby is ready to be born there is about a litre of amniotic fluid in the uterus.
The majority of amniotic sacs will burst during labour (‘waters breaking’, ‘membrane rupture’) because of pressure from the baby’s head and the cervix.
However, it is not medically necessary for waters to break in order for a baby to be born, some babies are born with the amniotic sac intact – known as being born in the caul.

“The hormones of labour are so important, they deserve a fanfare.
Labour is completely governed by the hormones and the fact is, nobody knows exactly why a woman goes into labour when she does.
We only know hormones are released from both mum and baby when both are ready for the process to start and they combine to make the most fantastic cocktail – one that’s capable of starting, progressing, completing labour and then providing everything mum and baby need once baby is on the outside” DD, 2020
IRONICALLY
ALL around the world, women are subjected to artificial versions of these hormones which, whilst they replicate the function of natural hormones i.e. cause the longitudinal muscles of the uterus to contract and pull up, they do not cross into the brain so do not trigger the pituitary gland to secrete all the additional hormones which give the emotional and mental support for the contractions, thus making labour so much harder than it needs to be.
Without that blood brain connection during labour, both mother and baby will be seriously lacking the necessary hormone production for the post-natal period.
Marsden Wagner Video on hormones of birth
There are loads of hormones involved in the main birth process and each has a vital part to play.
I like this from Dani’s book – “As with any production there are the main players”

 OXYTOCIN
OXYTOCIN
A.K.A ‘The Love Hormone
- Released when we make love, cuddle, stroke a pet, laugh, kiss, have a deep, meaningful conversation.
- It should be present for labour, giving birth, breastfeeding, bonding and attachment.
During labour and birth, Oxytocin causes:
- Uterine contractions to open the cervix
- Expansion of the birth canal alongside relaxation & opening of the p.f. (pelvic floor)
- Calming, analgesic effect (mum & baby)
- As labour progresses more is released, a natural augmentation (speeding up)
- A further surge during the last part of ‘active’ labour triggers the ‘foetal ejection reflex’ (pushing urge)
- released in pulses
- Contractions cause compression
- Pauses between these contractions
- The baby can lower their heart rate to cope with the reduced oxygen during a contraction, and, in the pauses, when there is no compression, the baby’s heart rate can recover. This process helps to squeeze all the fluid from the baby’s lungs, preparing them for when they are no longer connected to the umbilical cord.
-
The pressure of the baby on the cervix
-
Distension of the vagina
-
The fanning out of the pelvic floor muscles and the perineum
-
Stretching of the perineum as the baby’s head is crowning (being born)
-
Clitoral stimulation
-
Nipple stimulation
-
Skin to skin contact with the baby
Following birth
- Reduces stress outside the womb for mother and baby.
- Supports the start of breast feeding.
- Connects & primes those feelings of pleasure with the act of contact, holding, feeding and caring for the baby which encourages mutual bonding.
- Warms the front of the mother’s body through a process called vasodilation perfect place for the new-born, a new baby is not able to regulate their own body temperature.
- The Oxytocin receptors on the baby’s front absorb the hormone & help the baby feel less stressed as they nuzzle & look for milk, producing even more Oxytocin which encourages stronger, more effective contractions for the safe release of the placenta, thus reducing risk of a post-partum haemorrhage (excessive blood loss after birth)

 As you can see from this there are a number of processes and factors that trigger oxytocin at different points in the labour and I hope you are starting to understand the incredible physiology of birth, you’ll see how everything that happens does so for a specific reason. Therefore if we let someone intervene it interferes with the physiology.
As you can see from this there are a number of processes and factors that trigger oxytocin at different points in the labour and I hope you are starting to understand the incredible physiology of birth, you’ll see how everything that happens does so for a specific reason. Therefore if we let someone intervene it interferes with the physiology.
- The pressure of the baby on the cervix
- Distension of the vagina
- Fanning out of the pelvic floor muscles and the perineum
- Stretching of the perineum as the baby’s head is crowning (being born)
- Clitoral stimulation
- Nipple stimulation
- Skin to skin contact with the baby

Oxytocin is powerful BUT it is very sensitive & is threatened by fear, embarrassment, feeling observed, feeling cold, disturbances and loud noises.
It’s so important that a mother is left along during birth with as little disturbance as possible.
The first hour after the birth is vital so that the mother & baby have skin to skin. If the mother isn’t able to then the birth partner should be encouraged to.

- Medical procedures seriously interfere with the release of Oxytocin.
- Synthetic Oxytocin (Syntocinon or Pitocin (USA)) used induce or augment (speed up) labour
- Counter-productive
- Injected directly into the blood stream & ‘forces’ the uterus to contract, sadly the brain doesn’t get the feedback messaging to produce more natural Oxytocin (carrying its own analgesic effect).
FOR LABOUR PROGRESS
(without the usual hormonal support).
Hyper-stimulation of the uterus (no rest between contractions – hard for baby & mother) and the mother’s natural Oxytocin receptors can become de-sensitised.
Pain relief may be required & could result in prolonged pushing increasing the risk of an instrumental birth and/or post-partum hemorrhage.

An Epidural reduces the natural production of oxytocin in labour due to the numbing of the area which provides sensory feedback to the brain.
The catheter in the epidural space, used to administer the drug into the blood stream, also acts as a physical barrier to any neuro-messaging.
This can lead to labour slowing down, thus necessitating the use of Syntocinon; prolonged pushing; increased risk of instrumental birth and an effect on the bonding hormones.

An Elective Caesarean happens before the mother has gone into labour so neither mum nor baby receive any physiological pre-labour Oxytocin.
- It can impact on bonding due to the mother’s brain reward centres not being primed to respond to contact with her newborn.
- Oxytocin levels are not high enough to help reduce stress in mother and baby which can impact breast feeding.
- Baby is more likely to have respiratory issues because there have been no contractions to help prepare his lungs, so may require longer examination from the doctors and possible NICU care which of course impacts on skin to skin bonding.
- There is also an increased risk of a PPH (Post-Partum Hemorrhage).
If you delay your caesarean until nearer to 40 weeks then if you do go into labour this is beneficial for the baby. Squeezes the baby lungs stimulating the fluid in the lungs.
Caesareans carried out after the physiological onset of labour may have fewer negative impacts on Oxytocin production, although there are obviously certain elements which would still be affected.
Gentle Caesarean
Exploring all of your options and understanding what is involved in a gentle caesarean helps you to decide whether this is the option for you. The above video is one of our Ripple clients who negotiated the first gentle caesarean at Northampton General Hospital under the Consultant care of Dr Sara Dexter.
Here the client talks to me about the path to her choosing to request a gentle caesarean.
Birth Option – https://youtu.be/sjmv0gxr05I
What & How –
New Baby Smell –
Wow – https://youtu.be/YIUhTwf5kDg

An episiotomy (a cut into the perineum – the muscles surrounding the vagina and anus) will reduce its ability to stretch which further stimulates Oxytocin production.
Oxytocin production is absent if mum and baby are separated at birth.
So for those of you who have had a baby … I always ask my families who are having a second baby – what would you do differently this time especially if the choices were actually taken away previously … ?
This information is to help you understand the physiology of birth and, to appreciate how, left to do things on its own terms, how your body will do as it needs to.
It is so important to remember that whatever the circumstances of your baby’s birth, what you learn is going to help you to have a positive birth experience.

 Skin to skin is so powerful (regardless of how the baby is born).
Skin to skin is so powerful (regardless of how the baby is born).
As soon as you have the opportunity to hold and smell your baby
Spend as much time as possible, naked from the waist up, with an equally naked baby …
Inhale the smell of their head, even if it means delaying the onslaught of visitors for a while.
Skin to skin is not just for a new born, either.
Spend time skin to skin with your growing baby – bonding and re-connecting with them
Skin to skin is for both parents.
Skin to skin is for the other children or child it’s fabulous for their relationship.
The following is taken from Greys Anatomy where skin to skin or kangaroo care is described.

- Natural opiates in the body
- Potent
- effective painkillers.
- ‘floaty light’ feeling like all opiates
- hormone travels to the brain faster than any feelings of pain and blocks the pain receptors, so by the time pain signals reach the brain, the perception of pain is far less.
- The levels of endorphins in your blood stream are going to be higher.
- The high levels of amnesia-causing hormones are responsible for ‘baby brain’.
- In pregnancy, YOU are physically working hard – You are growing a human
- They increase towards the end of your pregnancy helps you prepare for the physical effort of labour
- You become more internally focused and tune into your baby.
- Endorphin levels increase during labour, a few days after birth, they drop back to pre-pregnancy levels as other hormones start doing their job, and this drop is often experienced as ‘the baby blues not to be confused with post-natal depression.
So, during labour and birth, Endorphins:
- Produce powerful pain-killers in response to the physical process of labour and the uterine contractions.
- Create a sense of well-being and promote positive feelings.
- Mother withdraws from the outside world, thinking brain increasingly internally focuses, she tunes into her baby and her body – more instinctive in her birthing behaviour.
- Amnesiac effect = women have memory gaps of their labour = natural reward for giving birth
Following birth:
- Prime the reward centres in the brain, making contact with and loving the baby a positive thing.
- Create a positive emotional climate for the first meeting with the baby.
- Provide a feeling of satisfaction and achievement with the birth which increases self-esteem and confidence.
- Lower stress in both mother and new-born, making the initial breast feed easier.
The Oxytocin produced in labour, encourages the increasing production of endorphins via the body’s feedback system.
Therefore anything that interferes with the physiological production of Oxytocin is also going to have a knock-on effect when it comes to the production of Endorphins.

- a stress hormone (part of the catecholamines family) – important in labour.
- The mother stays alert (despite Endorphin induced introverted state) aware of any potential danger.
- Important for baby – a late labour rise in Adrenalin helps them cope with the intense contractions before birth.
- It preserves blood flow to the baby’s heart and brain and helps to clear the lungs of fluid, preparing them for the outside world.
-
Encourages a level of alertness and energy in the baby after birth, so they can initiate and take full advantage of their first feed.
-
The sharp drop in levels encouraged by skin to skin after the birth maximizes the efficiency of the contractions in expelling the placenta with minimal bleeding.
-
Conserves energy in the baby ensuring they don’t fall asleep before taking enough nourishment.
But too much Adrenalin can totally de-rail the whole labour process.
- produced as an important element to our ‘fight or flight’ response, the essential part of our ability to survive in the face of danger.
- If we are in a life-threatening situation, feeling loved up and floaty light isn’t going to be helpful.
If the mother feels threatened, frightened, exposed, anxious, cold or all the above in labour, Adrenalin will kick in, reducing the production of Oxytocin and Endorphins.
Too much Adrenalin in the context of birth is not going to be helpful.

- Relaxin softens & relaxes the ligaments & muscles of the pelvis & perineum to make them soft & stretchy.
- Inhaling oxygen during labour = higher levels of Relaxin, enabling the birth canal to soften and widen.
- The baby rocks their head back and forth over the perineum as they are crowning, it encourages even more Relaxin to be produced, ensuring those muscles to open softly and gently = minimising the risk of tearing. Encourages Oxytocin production for the next stage of the motherhood/birth journey.
- Directed Pushing = higher risk of tearing (i.e. being instructed on how and when to push), because levels of Relaxin aren’t given the necessary time to build up in the blood stream.
- During pregnancy, the Relaxin can also be responsible for pelvic pain sometimes known as Symphysis Pubis Dysfunction (SPD) or Pelvic Girdle Pain (PGP) because it can make the ligaments too soft, stretchy and moveable.

- responsible for ripening the cervix
- Switches on the Oxytocin receptors in the uterus = receptive to the Oxytocin being released and causing contractions.
- When you are offered a ‘stretch and sweep’ near or after her due date, the idea is to irritate the membranes of the cervix to encourage the Prostaglandins to rush in and start the process off
- Semen is a natural carrier of Prostaglandin = making love is considered a sure-fire method of starting labour if the baby & body are ready. It’s fun trying if you can find a comfortable position.
Melatonin – is produced when it’s dark. Brain receives messages from the eyes – produces melatonin – we feel sleepy
This is relevant to labour because Melatonin boosts Oxytocin and if it’s dark, we feel less exposed and more relaxed.
Are you starting to understand why interventions, your environment and other events surrounding birth can cause problems for the labour journey … it’s a finely tuned process that requires balance. I can’t emphasis enough you need to know your options and choices.

The process of birth is purely physiological.
It ebbs and flows, stops and starts, peaks and troughs, and basically moves to its own rhythm.
Fear surrounding birth and the powers that be do measure birth so they can assess when to intervene. Intervention is sometimes necessary and in some cases, will save lives,
Interventions happen because hospital guidelines, policies and protocols drive it rather than it being necessary for the individual.
Birth is nothing like the media depicts it to be …
- Progress based on how dilated the cervix is
- Cervix dilated 4 – 5 cm = ‘established’ labour. The new 6cm
- This is just snapshot of information, it shows what is happening at that particular moment – Doesn’t tell you what has or will happen
- Reed, (2015) cervical examinations only happened if labour wasn’t progressing and they needed to confirm it.
- NOW cervical examinations are ‘offered’ routinely every 4 hours.
- When do I go in? Some will often end up going in far too early = unnecessary intervention or being sent home.
- A partogram plots the progress of labour ( ‘The Friedman’s Curve’, (1950)) requires a vaginal examination, to check cervical dilation If not dilated 4cm or more = being sent home unless there has been an event.
- Admitted you are expected to dilate an average ½ cm per hour. VE every 3-4 hours to check progress. If slow progress or no change labelled ‘failure to progress’ which will then ‘require’ intervention. Fear Tension Pain
- A large study in 2010 (Zhang J et al) 62,500 maternal records, research found a wide variation in cervical dilation. The average women began active labour at 6cm and the average time it took to dilate during active labour was about ½ cm per hour. Despite the research, the original Friedman’s Curve is still used.

Labour has three stages:
First stage – this is where the cervix softens, thins and dilates to 10 cm. The first stage is split into the latent phase, early labour, established or active labour (considered to be 4cm).
Second stage – this is when the uterus starts to push out the baby. Second stage starts when the cervix is dilated to 10 cm
Third stage – this is the delivery of the placenta
But as you know, real life is not a textbook and every woman is different.
FOCUS on birth physiology – understand, trust and listen to your body.
Stay home for as long as you can (if birthing in hospital or birth centre) obviously transfer in when you feel YOU need to. Slightly different if you are booked in due to an intervention or you plan to stay at home.
- Cervical dilation is only part of the picture
- The cervix is dilating the muscle mass is gathering on top of the fundus (this helps push the baby down & out)
- Vaginal Examination may not look like it but it’s always doing something
- Be aware of emotional and behavioural changes, keep an eye on what is going on with the contractions, as this usually provides a much more accurate assessment
- A mother will go through 3 major emotional stages as labour progresses.
These behavioural changes are all to do with the hormones of labour. When a woman is calm and feels safe, her body naturally takes her from one stage into the other.
Excited Mama – Keep doing normal activities Set yourself a pre-birth project Set the scene Inform those that need to know Stay at home
- Early/latent stage of labour.
- Contractions can stop, start and be irregular. How long is a piece of string – who knows.
- Be able to talk through your contractions (especially the early ones)
- If you partner talks to you, you’ll be able to make eye contact with them.
- Be able to speak in full sentences and hold a proper conversation.
- If you have to stop because of a contraction, once it’s finished, you’ll be able to resume the conversation.
- Labour can start at night (Melatonin boosting Oxytocin)
- Women will, most likely, be in their own environment, with their partners, curled up in bed feeling relaxed and sleepy.
- if partners are away or working a night shift, their bodies will tend to wait until daytime to start the process off.
- Mothers of older children, labour won’t kick in until the older child/children have been taken care of.
- If you’re asleep and the contractions wake you, pop on the TENS and go back to bed!
- Distraction – box sets, 2000-piece jigsaw puzzles, going for a walk
- Conserve energy; sleep, eat and rest as much as possible.
- Take a nap/bath – especially if contractions stop, rest over a ball, or over cushions piled up on the sofa and nap in between.
Serious Mama
- Oxytocin increases as labour progresses
- Contractions become longer, stronger and closer together (or should)
- Focused on your contractions USE YOUR breathing and relaxation techniques.
- Rest between contractions
- Your ability to talk will decrease, gradually become more and more monosyllabic.
- Contractions get stronger, the Endorphins help you cope
- Partner matches your mood. If you’re not talking, don’t engage her to disengage, offer a drink or a massage, don’t wake up the neo-cortex
- Oxytocin levels increase, contractions intensify, move with each one.
- Behaviour is likely to become repetitive, the 3 R’s – IF IT ISN”T BROKE DON”T FIX IT
- Noise with your out breath, a noticeable exhalation every time you breathe.
- Waters may break and you may start to lose your inhibitions.
- Subsequent babies can be a bit quicker and you’ll obviously need to factor in how far away you’re from hospital and whether it’s rush hour or not.
3 – 4 long, strong contractions, lasting at least a minute, within a 10-minute period, happening consistently for an hour!
Contractions lasting around 45 – 60 seconds
Contractions around 3-5 minutes apart – increase in strength and intensity of contractions,
Focus on breathing, letting your body go completely limp
“Do not disturb” sign
Could last many hours
Some women’s contractions never get this close (stronger & longer)
Doubtful Mama – Final part of the first stage
- Commonly known as transition – adrenalin fueled – journeying deeper into labour – she is safe.
- Be ‘high’ on the Endorphins – might be ‘other worldly’. The boost of Adrenalin cancels out (or lessens) the floaty effect of the Endorphins to ensure you’re alert enough to greet your baby and keep it safe.
- Aware of the double-peaking contractions it may feel there are no breaks between them.
- May become very vocal – shouting or making loud ‘mooing’ noises, some will say they’ve changed their mind about having the baby and want to go home, some will remain extremely quiet and her supporters will have no idea of the turmoil within, some will become needy and some will display signs of utter panic.
- Flushed, nauseous or be sick, you could be shaking, vocalizing – “I’ve changed your mind” “I want to go home”
- All to be expected – positive sign – need encouragement & reassurance
- This can be alarming for some partners – it’s all completely normal
Contractions are much more intense.
Can happen around 7cm as well as 10 cm (with mini self-doubt at earlier stages of labour) “Don’t Know if I can do this”.
Extra encouragement, praise and support.
Physical responses – shaking, nausea, hot flushes.

- I love the “Rest & Be Thankful” stage
- The contractions may slow down, perhaps they hit a pause or they stop completely.
- You have journeyed the most intense contractions; now is an opportunity to rest & recover
- Baby’s head has opened the cervix fully and waiting for the messages to produce more Oxytocin for contractions to move the baby into the birth canal
- You may even SLEEP – YES you could
This is not a time for anyone to try and rush this or force anything to happen.
Rest, Eat, Drink, Wee, Breathe, REPEAT or SLEEP

Foetal Ejection Reflex
- Pressure is applied to the nerves deep in the pelvis.
- The uterus does the work, the body is doing it by itself, making the contractions increasingly expulsive, and the mother starts to feel the urge to bear down.
- An increase in Adrenalin provides the energy to birth (push) the baby out, to be alert to greet them and spontaneously fall in love (sometimes this doesn’t happen).
- Grunting & “pushy” noises.
- Listen to your body and don’t be de-railed by being given instructions (Directed pushing – “hold breath & push, push, push”, “Push into your bottom like you’re doing a poo” NO PURPLE PUSHING – cutting oxygen to baby & yourselves.
- No urge don’t force it – WAIT there is NO RUSH (Simpson, 2006).
- Directed or coached pushing is more likely to cause tears, distress in both mother and baby and result in an instrumental delivery (Reed, R; 2016.)
- Eyes may be closed and should not be interrupted.
- Room needs to be kept dark and quiet, no room for neo-cortex activity here!
- ‘listen to your body’ and do what feels right.
- Baby moves down, soft tissues stretch, Oxytocin is released.
- May need a poo due to the baby’s head in the birth canal, to the back passage.
- Poo is a positive as closely followed by a baby’s head

This section is for the Birth Partners … for those that might be with you so that they can understand what they might be hearing / seeing …
- contraction pattern becomes increasingly stronger & powerful
- eyes closed and doze between contractions – in their own world – may even cover their eyes or hide their head
- Less able to respond to questions (DON”T ENGAGE THE NEO-CORTEX) – Abrupt answers – Water!
- Movements and sounds will be instinctive and rhythmical – Vocalise during contractions – often the same noise with each one, and/or make the same movements each time.
- Inhibitions are reduced. Naked – the hormonal symphony is in full swing
- Baby moves down and pelvis becomes less stable (opening), posture changes.
- Hold onto things (and people) when standing/walking.
- Will not be able to sit directly on her bottom.
- Walk leaning slightly with a ‘waddle’ as the pelvis tips.
- Transition may see fear – give reassurance and support (some don’t)
- Adrenaline during transition can cause a dry mouth and she might suddenly be very thirsty. – High levels can also cause vomiting as the stomach empties in the fight or flight response.
- Cervix opens to its full capacity you might see a bloody/mucous show and the waters break.
- May be a ‘rest and be thankful’ phase after transition where contractions slow and the woman rests as the baby descends into her pelvis.
- Pressure in her bottom, or that she needs to poo. May be poo as the baby compresses the rectum and squeezes it out.
- Contractions become expulsive and pattern changes.
- Noises and behaviour also change.
- Visual signs of the baby’s head descending in her perineum – gaping anus and vulva, flattened perineum, bulging bag of waters (if still intact), the baby’s hair/head, etc.
- As the baby’s head stretches her perineal tissue she will hold back her pushes, gasp, scream, close her legs, and/or hold her baby’s head in
- Baby’s head is born you may see them rotate or wriggle then be born with the next contraction (there should be some movement or change with the next contraction). (Reed, R; 2017)

Skin to Skin
- Placed on you or you bring baby to you
- Golden Hour
- Regulates baby’s body temperature, breathing, blood sugars, heart rate
- Safe place so reduces stress hormones in both mummy & baby
- If plan to breastfeed skin to skin, baby instinctively looks for food
- Placenta is birthed – if physiological, uninterrupted birth the period between the birth of the baby and the birth of the placenta is important. Umbilical cord contains 1/3rd of the baby’s blood volume which if they are still attached they will get it is rich oxygenated blood. (See the video in the Umbilical Cord area).
- Increased oxytocin levels from the skin to skin helps the uterus contract
- Placenta peels away from the uterine wall
- Blood vessels interwoven in the muscle fibres of the uterus. These fibres act like a ligature to stem the bleeding.
- Physiological – more initial bleeding but less over the following weeks
- Managed – ergometrine (intramuscular injection) massive contraction & expels the placenta. Midwives may massage the top of the placenta and apply gentle traction on the cord. Less initial bleeding but more over the following weeks.
Higher chance of a retained placenta. Cervix closes with the placenta still inside which then results in a surgical procedure under epidural/spinal to have it removed - If the birth involved intervention or was particularly long or rapid or there was an issue with bleeding (normal blood loss is estimated to be around 500ml), a managed third stage would be advised.
- Whichever third stage you choose, the cord will ideally be left to pulsate for as long as possible, and will preferably be empty. The NICE (National Institute of Clinical Excellence) Guidelines (2014) state it should not be clamped before at least one minute unless there are indications you or your baby need some help.
- You’ll bleed for a few weeks after birth regardless of how you gave birth because the additional womb lining that made carrying a baby possible has to come out. This bleeding is known as lochia and, depending on whether you had a physiological or managed third stage, can vary in the length of time it takes for bleeding to stop. Pay close attention to any blood clots.
- if you notice any foul smelling discharge or just feel unwell – all could be indicative of retained placenta which will need to be removed.

Every woman is different and may not show any of the following it does not mean she’s not in labour.
‘Optimum’ position i.e. Occiput Anterior (OA) which means their chins are firmly tucked into their chests and they are on their mother’s left side with their spines slightly angled towards the mother’s front. Occiput Posterior babies (OP) i.e. those which have their backs to their mother’s backs and the head is often de-flexed, have different methods of getting through the pelvis. Have you mapped your baby?
Mother’s with OP babies may have very intense contractions from the beginning with little or no dilation, they can experience early transitions (self-doubt) and may feel the need to start pushing early. In these circumstances, it is even more important that these mothers are encouraged to listen to their bodies and adopt positions that feel right for them, and in many ways, disregard the conventional forms of assessing labour progress because they often don’t apply.
So, some of these you may want to share with your birth supporters, or some of you may just want to inform your own learning.
- Sounds of Birth
- Smell
- Another show
- The purple line
- Physical Make-up
- Height of the fundus
Sounds of birth
Definite ‘birth’ noises that accompany the different stages of birth.
- Early labour (Excitement) the mother will be able to chat as normal;
- Established labour (Serious) she is going to find it more difficult to talk and there will be a few noises – as in focusing on the out breath;
- nearing the end of the first stage as she gets closer to Transition (Self-doubt) the noises will be loud humming and groaning.
- When she starts to push, it is often accompanied by grunting noises. However, some women are very quiet, and often those that are ‘hypnobirthing’ make no or very little noise so don’t rely on this method alone to assess progress.
Smell
There is a certain smell that is emitted as a woman gets nearer to birth. It is incredibly difficult to describe but it is ‘earthy’, ‘powerful’, ‘musky’. It’s one of those things you need to smell a couple of times before you think – ‘Ah, now I know what she’s talking about.’
Another show
Regardless of whether a woman had a ‘show’ at the start of her labour, the act of giving birth does involve copious amounts of bodily fluid – blood and mucous being very likely. They are often released during contractions when the mother is around 6 – 8 cm. This is often the time the waters will go and if they broke earlier, there is often another gush at this point.
 The purple line
The purple line
I have seen this a few times depends on the position the mum is in and the colour of her skin.
The purple line starts just above the anus and grows up the natal cleft (or bottom crack) as labour advances, a bit like the mercury in a thermometer.
The length of the line is equivalent to how many cm the cervix is dilated!
Aren’t we amazing
Physical make-up
Physical occurrences that can indicate a woman is 6cm or beyond.
- Involuntarily curling her toes during contractions, even when the rest of her body is totally relaxed.
- If standing she may stand on her toes whilst leaning over something.
- Goose bumps may appear on her bottom or upper thighs.
Height of the fundus
When the uterus contracts it moves upwards and pulls the cervix upwards with it which is what causes the dilation.
At around 40 weeks of pregnancy, it should be possible to get 5 finger widths between the top of the bump and the very bottom of the breastbone – kind of that upside down ‘V’ between your ribs. As the mother dilates, that space between the two points is going to lessen until the cervix is fully dilated and it is no longer possible to get any fingers in between the two points.
However, this method is much more relevant to women who have had previous babies and, unfortunately, the measurement has to be taken at the peak of the contraction when the mother is lying flat on her back.
This summary sheet will be really helpful for your birth partner(s)
Updated Partners handout copy

“I feel absolutely gutted about how things turned out. I’m annoyed with the HCPs for not supporting me but more than anything I’m annoyed with myself for not having faith in my body and for allowing myself to be manipulated by the HCPs into following their preferred pathway. I won’t ever get to experience physiological birth now or the healing birth that I needed so much. I don’t know how to get past this – maybe it’s too soon to even think about getting past it? I don’t feel ready yet to start processing what happened.”
The Performance Link
Mama Goddess – Willow’s Home Birth Link
Push it Real Good Link
Links:
Acknowledgements:
Dani Diosi – Hynobirhting – Breathing with Short Pants
The Student Midwife Student


















